Soap Note Pediatric Example A pediatric SOAP note is a structured format for documenting a patient s medical information in a concise and organized manner SOAP stands for Subjective Objective Assessment and Plan and each component of the note serves a specific purpose
Learn how to write pediatric SOAP Notes Included are examples from SLPs that work with a pediatric caseload including articulation soap note examples Denies fever No chills No night swears Theree is no unexplanined weight loss Patient does not have associated sinus congestion runny nose sore throat chest pain wheezing or dyspnea He has tried no medicaitons for relief of symptoms He has no current or past smoking exposure
Soap Note Pediatric Example

Soap Note Pediatric Example
https://i.pinimg.com/originals/90/84/00/908400d66a6a5e25d3edc337a39141e8.jpg
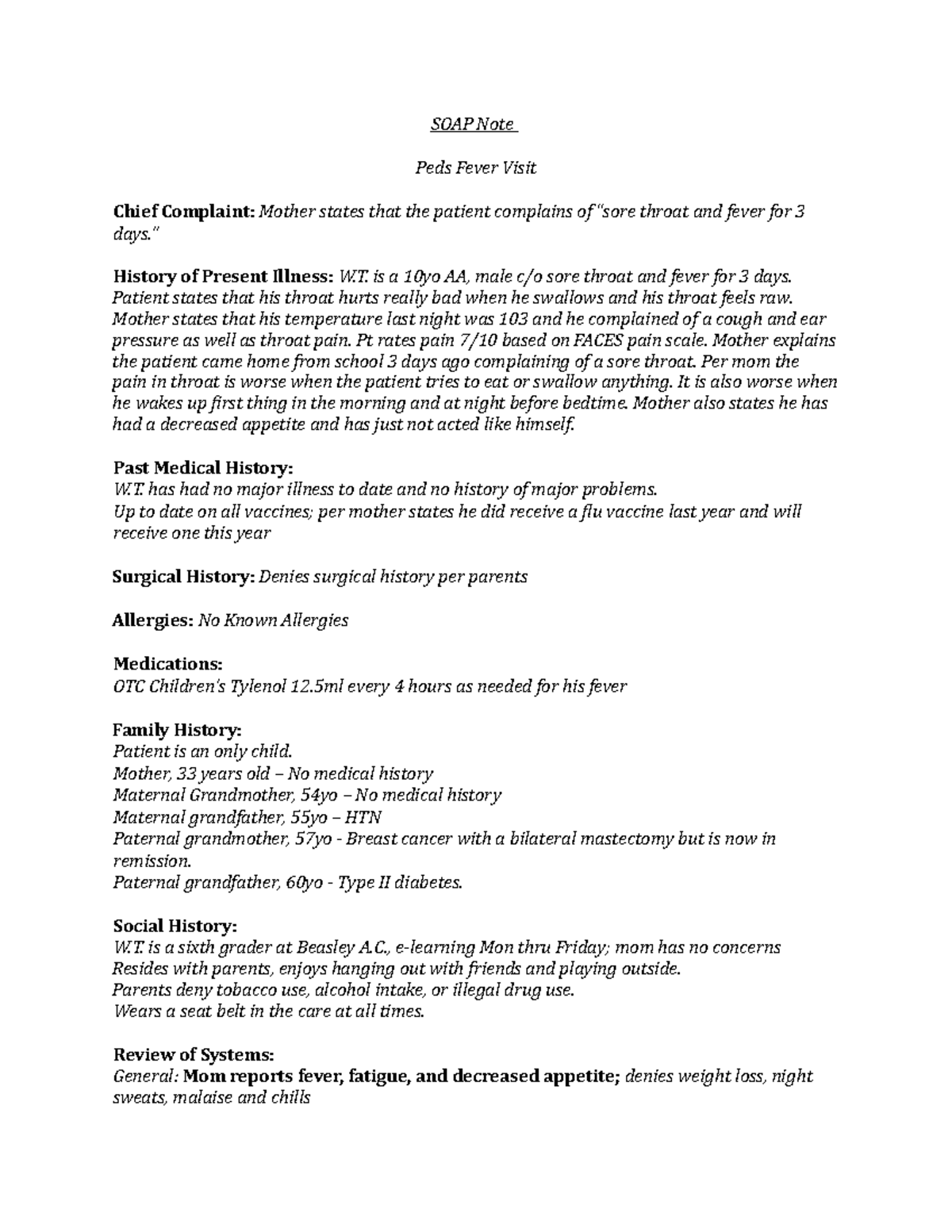
Peds Fever Soap Note SOAP Note Peds Fever Visit Chief Complaint
https://d20ohkaloyme4g.cloudfront.net/img/document_thumbnails/ee112f3820e5e7994ca3f6f767ce7960/thumb_1200_1553.png
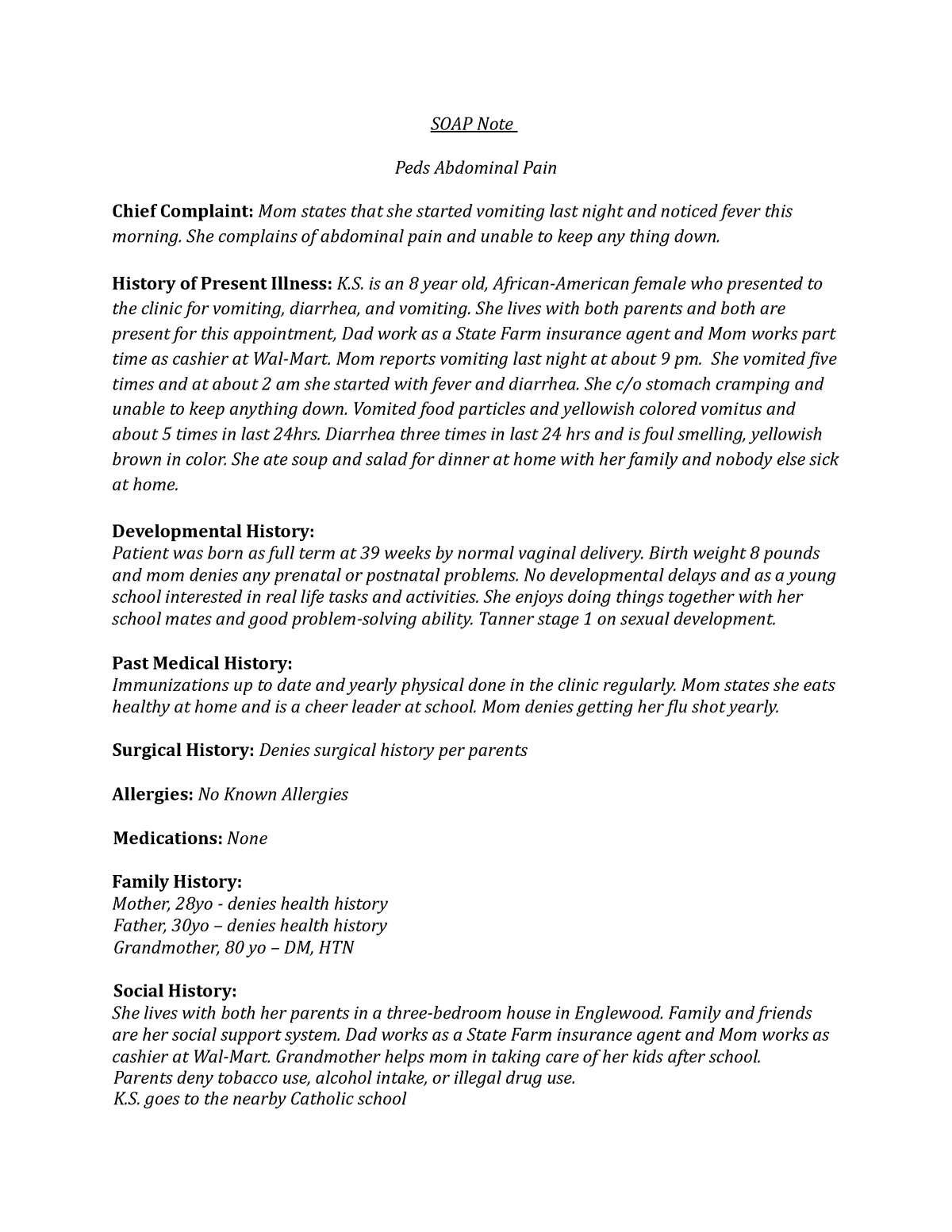
Peds Abd Pain Soap Note SOAP Note Peds Abdominal Pain Chief
https://d20ohkaloyme4g.cloudfront.net/img/document_thumbnails/73f811bd16710808c396ebcad2d20ef7/thumb_1200_1553.png
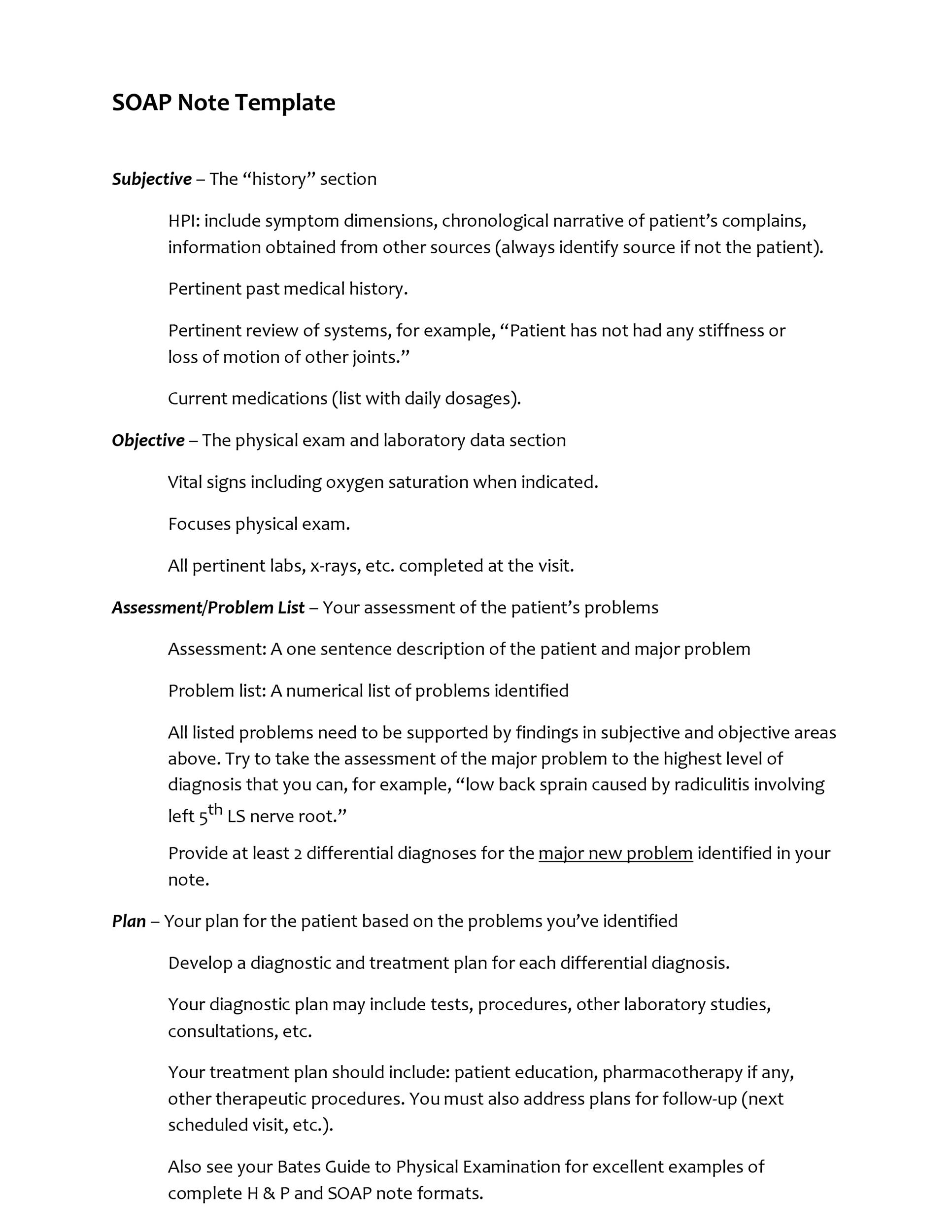
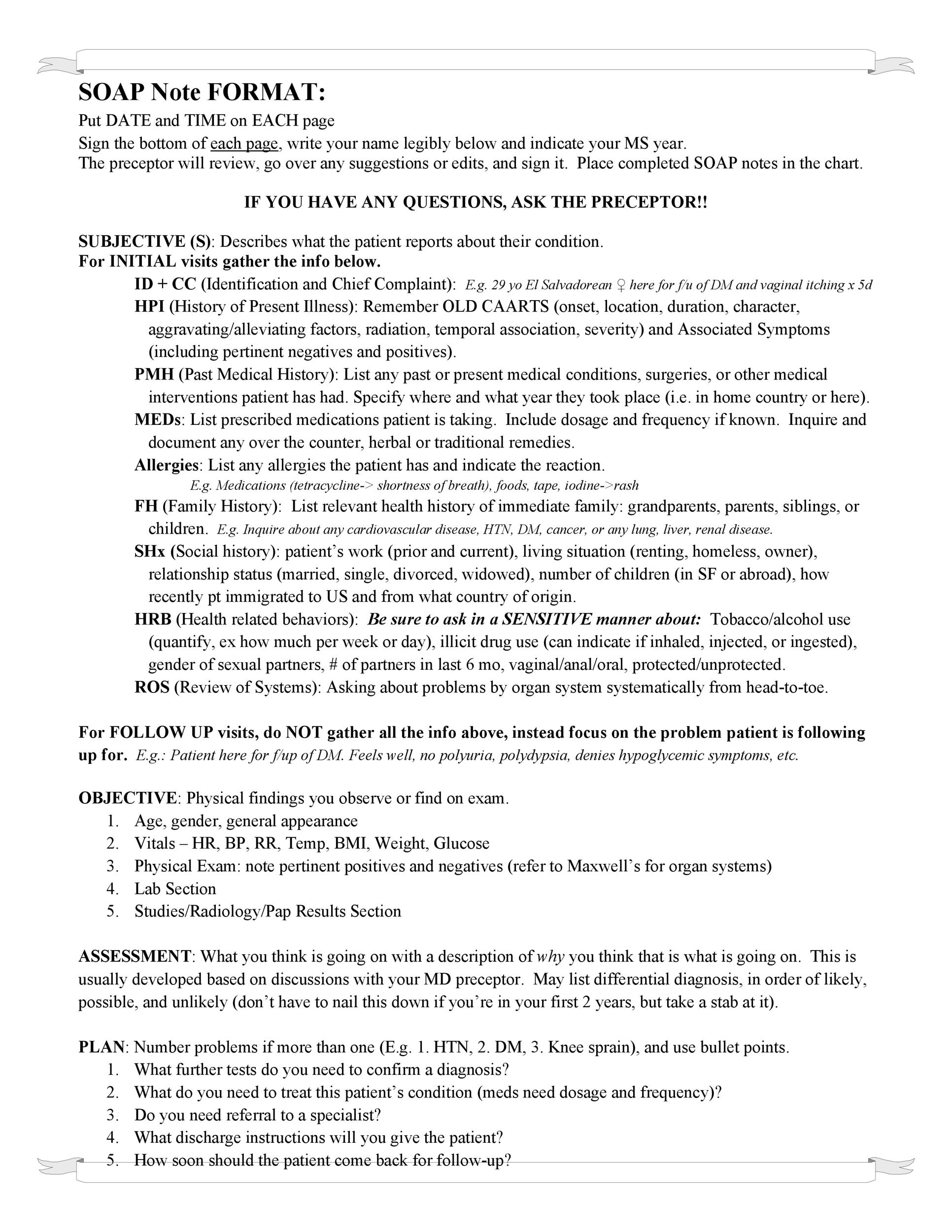
Here are examples of each section of a good SOAP note S Subjective Your impressions of the patient s level of awareness mood and behavior You can also include direct quotes from the patient This is a good place to include how a patient feels about their speech improvement or therapy in general 1 Create daily notes with a consistent structure and flow Having a standard yet versatile daily SOAP note template that you can use for every appointment ensures that you are presenting a consistent flow of easy to interpret information to your readers and reviewers
Here s info on pediatric SOAP notes including pediatric SOAP note examples which will be helpful for those in pediatric behavioral health Pediatric SOAP Notes are a method of documentation used by healthcare professionals to record the details of a child s medical encounter SOAP an acronym for Subjective Objective Assessment and Plan provides a clear and organized structure for noting crucial aspects of the patient s status and the treatment plan Challenges of Pediatric Notes
More picture related to Soap Note Pediatric Example

Pediatric Soap Note Example Nurse Practitioner Sharedoc
https://i.pinimg.com/736x/f5/71/ef/f571ef9de9caf7dc92087d6311ac4294.jpg
40 Fantastic SOAP Note Examples Templates TemplateLab
https://templatelab.com/wp-content/uploads/2017/04/Soap-Note-Template-01.jpg

Pediatric Soap Note Template Awesome 15 Soap Note Examples Free Sample
https://i.pinimg.com/736x/42/a2/c8/42a2c85075dbcb8a98c39b696c44b7bf.jpg
Pediatrics Top 10 Neurological Exam By SOAPnote posted 2010 04 01 updated 2019 12 22 Neurology Objective Exam Elements Structured Data Index 0 78 approximately 182 views in the last month Favorite 14 Headache History By SOAPnote posted 2017 12 22 updated 2019 12 22 Neurology Subjective History Elements Tags migraine A pediatric SOAP note is a type of progress form used by pediatricians nurses and other healthcare professionals when assessing the health of a child It is based on the acronym SOAP which stands for Subjective Objective Assessment and Plan The note includes information gathered from the patient and or parent physical exam findings
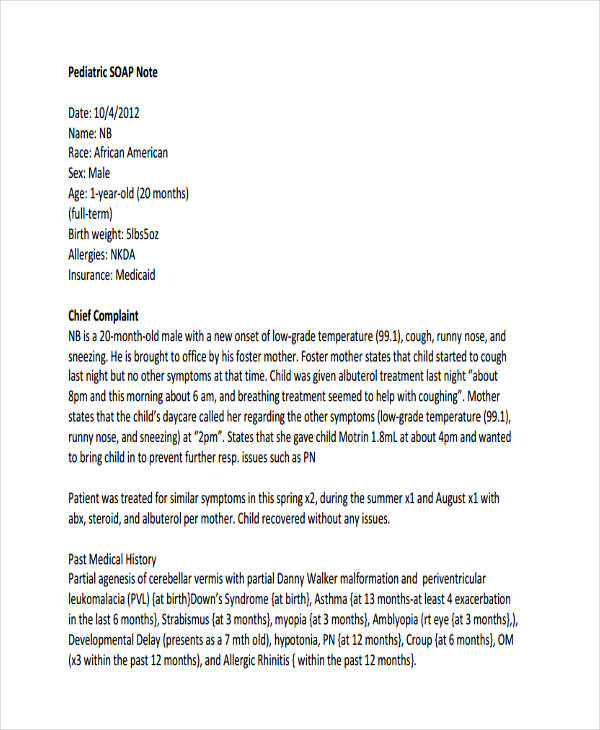
General Pediatric Exams By SOAPnote posted 2010 11 26 updated 2023 02 22 Noteworthy Objective Exam Elements Pediatrics Cite Favorite 29 approximately 294 views in the last month View Skin Normal turgor and without lesions Eyes Red reflex present bilaterally Pupils equally round and reactive to light Pediatric SOAP Note Date 10 4 2012 Name NB Race African American Sex Male Age 1 year old 20 months full term Birth weight 5lbs5oz Allergies NKDA Insurance Medicaid Chief Complaint NB is a 20 month old male with a new onset of low grade temperature 99 1 cough runny nose and sneezing He is brought to office by his foster mother
40 Fantastic SOAP Note Examples Templates TemplateLab
https://templatelab.com/wp-content/uploads/2017/04/Soap-Note-Template-23.jpg
SOAP Note Examples 19 In PDF Examples
https://images.examples.com/wp-content/uploads/2017/04/Pediatric-SOAP-Note.jpg
Soap Note Pediatric Example - Pediatric SOAP Notes are a method of documentation used by healthcare professionals to record the details of a child s medical encounter SOAP an acronym for Subjective Objective Assessment and Plan provides a clear and organized structure for noting crucial aspects of the patient s status and the treatment plan Challenges of Pediatric Notes