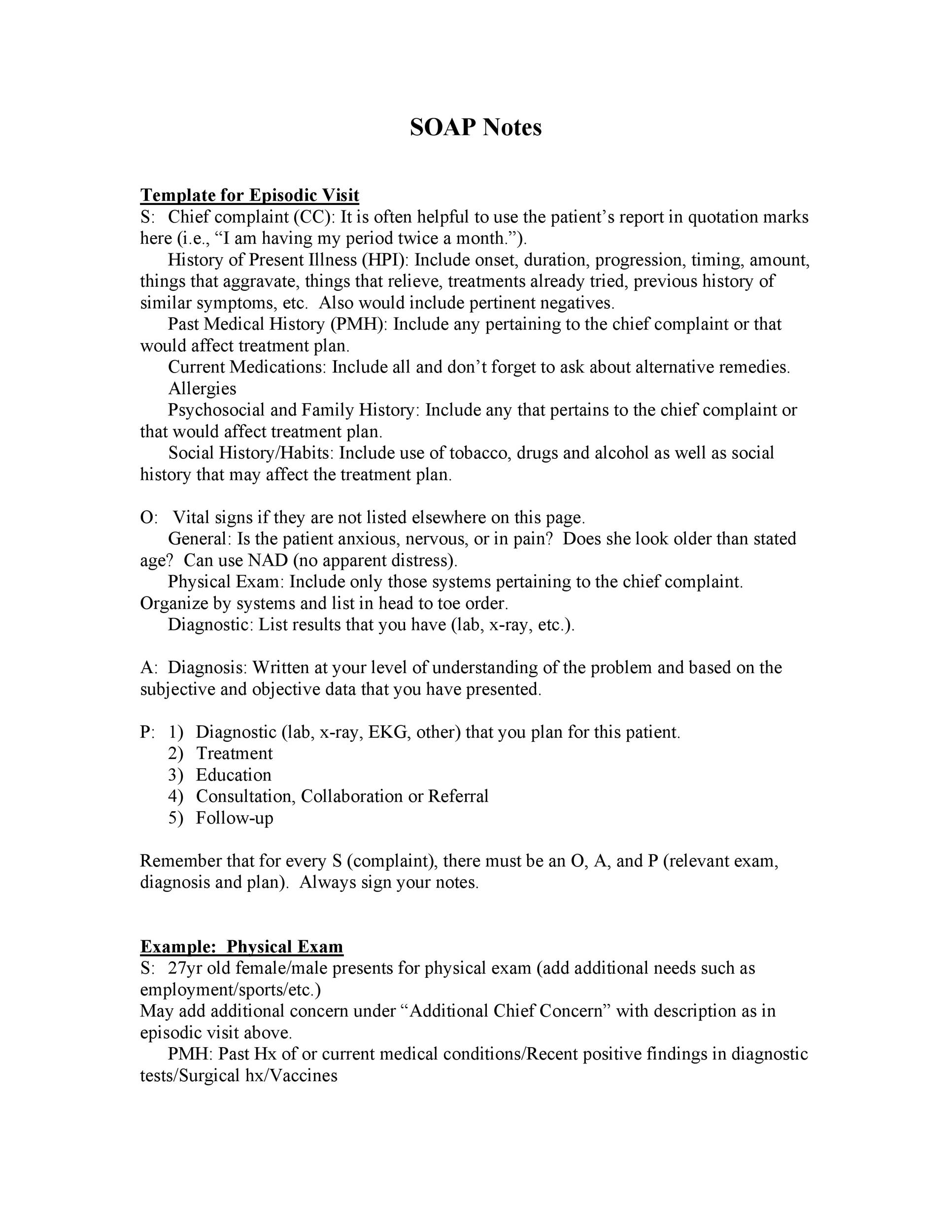
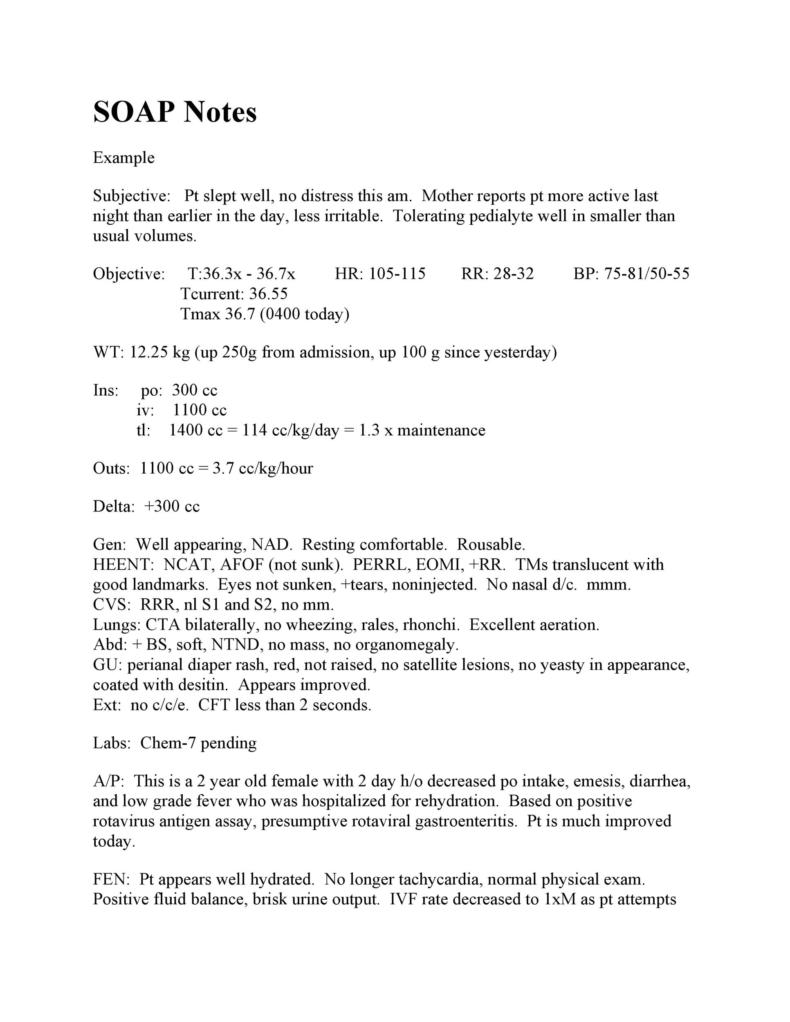
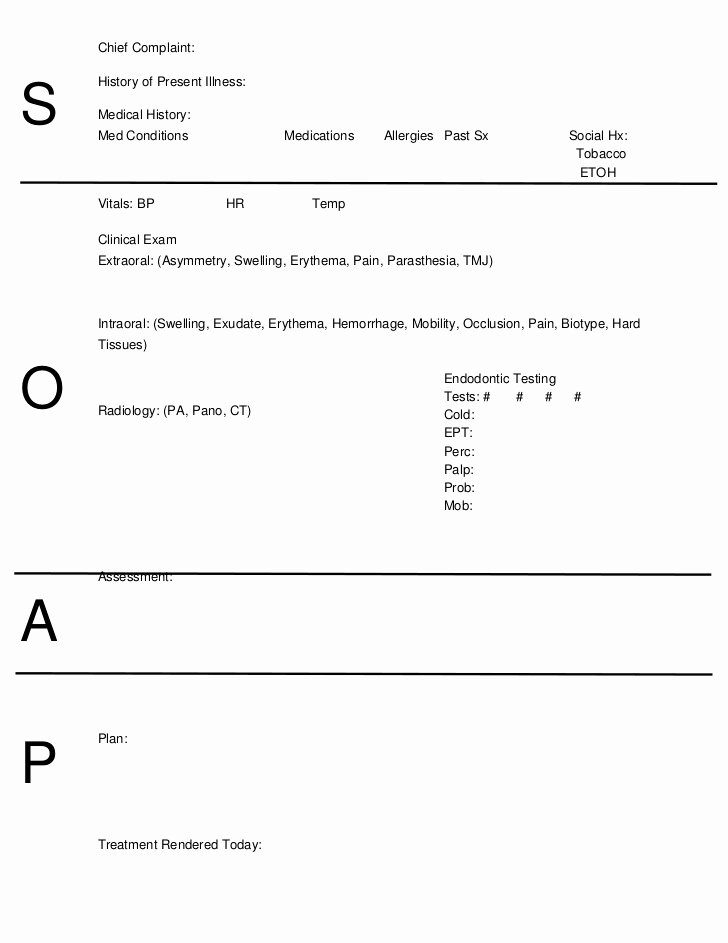
Sample Pediatric Soap Note What is a Pediatric SOAP Note A pediatric SOAP note is a structured format for documenting a patient s medical information in a concise and organized manner SOAP stands for Subjective Objective Assessment and Plan and each component of the note serves a specific purpose
Learn how to write pediatric SOAP Notes Included are examples from SLPs that work with a pediatric caseload including articulation soap note examples Pediatrics Top 10 Neurological Exam By SOAPnote posted 2010 04 01 updated 2019 12 22 Neurology Objective Exam Elements Structured Data Index 0 78 approximately 182 views in the last month Favorite 14 Headache History By SOAPnote posted 2017 12 22 updated 2019 12 22 Neurology Subjective History Elements Tags migraine
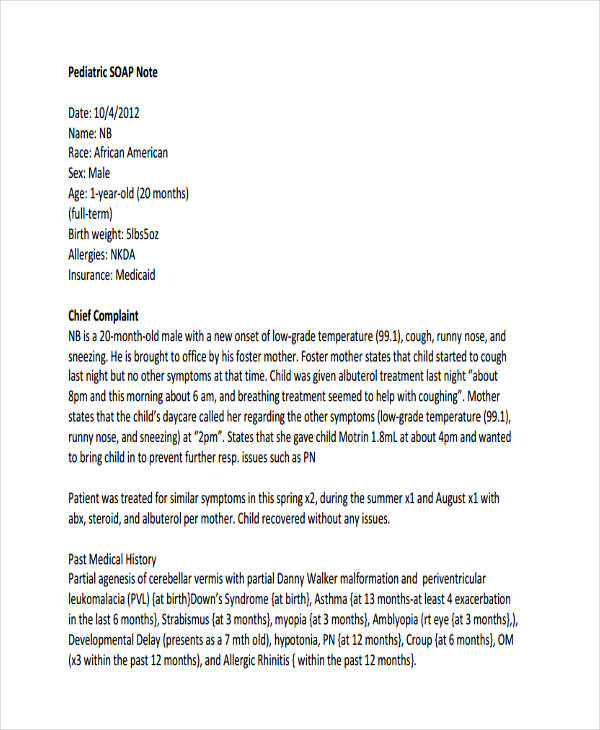
Sample Pediatric Soap Note
Sample Pediatric Soap Note
https://templatelab.com/wp-content/uploads/2017/04/Soap-Note-Template-26.jpg
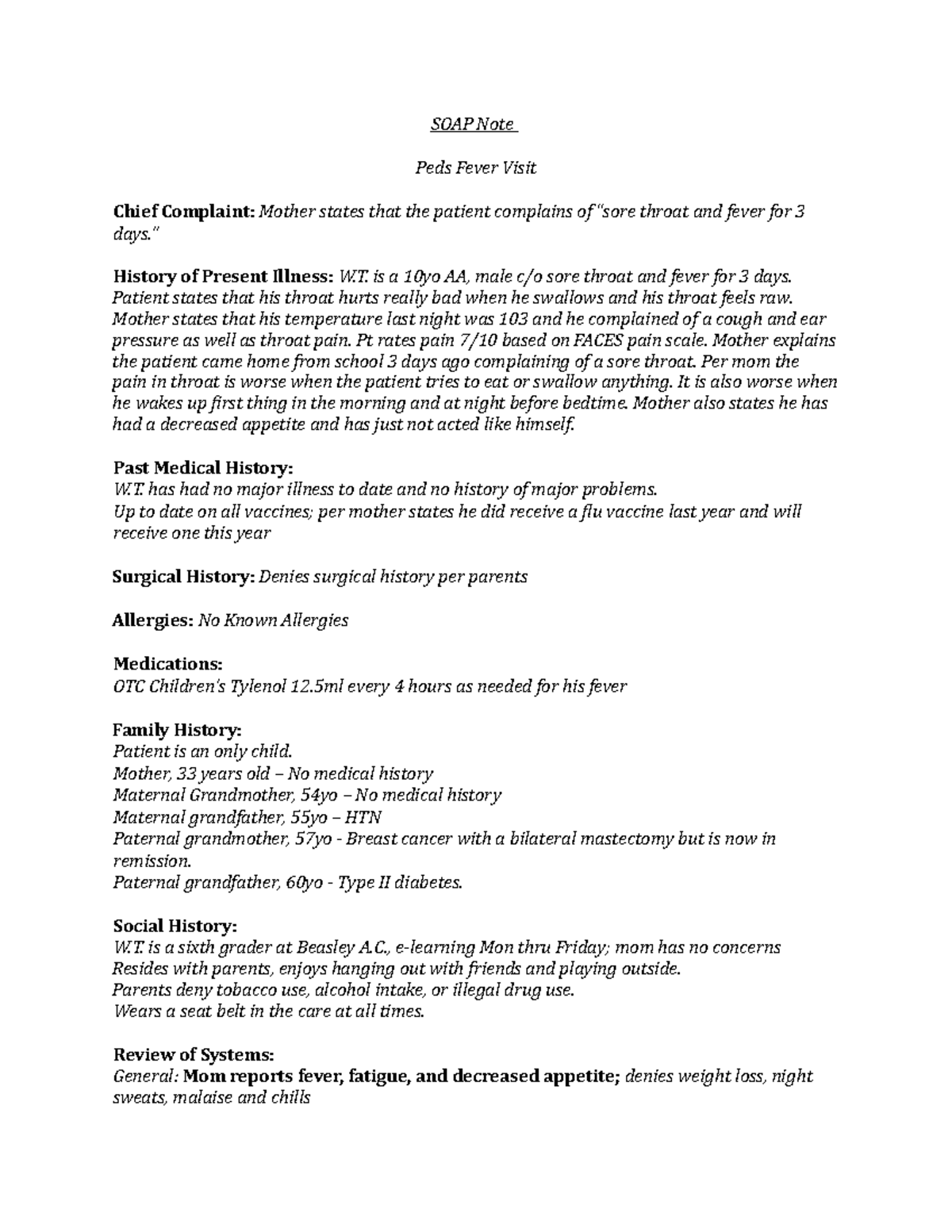
Peds Fever Soap Note SOAP Note Peds Fever Visit Chief Complaint
https://d20ohkaloyme4g.cloudfront.net/img/document_thumbnails/ee112f3820e5e7994ca3f6f767ce7960/thumb_1200_1553.png

47 Infant Soap Note Example Images Nalo
https://i.pinimg.com/736x/aa/5d/fa/aa5dfab83bef445d68ddc9906613af30.jpg
Here s info on pediatric SOAP notes including pediatric SOAP note examples which will be helpful for those in pediatric behavioral health A Assessment Your analysis of the session If possible compare the patient s performance across sessions EXAMPLE Suzy s correct production of k in initial position increased from 60 in imitation and with a visual aid during the last session to 70 during today s session
1 Create daily notes with a consistent structure and flow Having a standard yet versatile daily SOAP note template that you can use for every appointment ensures that you are presenting a consistent flow of easy to interpret information to your readers and reviewers A Full Guide DataMyte Pediatric SOAP notes are an effective way to track patient progress in the pediatric setting They provide detailed information that can be used for diagnosis treatment planning and follow up care In addition by utilizing a standardized format doctors can ensure accuracy when collecting and documenting essential
More picture related to Sample Pediatric Soap Note

Image Result For Surgical Notes Sample Soap Note Notes Template
https://i.pinimg.com/originals/bd/be/84/bdbe8452358603ea92f9be77fce38c14.jpg
40 Fantastic SOAP Note Examples Templates TemplateLab
https://templatelab.com/wp-content/uploads/2017/04/Soap-Note-Template-38-790x1022.jpg
40 Pediatric Soap Note Template Markmeckler Template Design
https://markmeckler.net/wp-content/uploads/2019/11/pediatric-soap-note-template-fresh-soap-notes-dentistry-word-of-pediatric-soap-note-template.jpg
A pediatric SOAP note is a type of progress form used by pediatricians nurses and other healthcare professionals when assessing the health of a child It is based on the acronym SOAP which stands for Subjective Objective Assessment and Plan The note includes information gathered from the patient and or parent physical exam findings Complete SOAP Note PEDIATRIC Student Sheri Harrison Course NURS7446 Fall 2014 Date 11 22 2014 Patient Select Patient Setting Selma Pediatrics Acute Care Primary Care SUBJECTIVE DATA I Identifying Data A Initials NM Age 8 YEARS DOB 03 25 2006 Sex Male Race Ethnic Origin African American B Informant Mother and Patient
Introduction SOAP notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes Using a template such as SOAP note means that you can capture store and interpret your client s information consistently over time SOAP note guide to the comprehensive pediatric write up instructions for use of the section on pediatric history and physical exam the following outline for the Guide to Pediatric SOAP note Course Advanced Health and Physical Assessment Across the Lifespan MSN572 61 Documents
SOAP Note Examples 19 In PDF Examples
https://images.examples.com/wp-content/uploads/2017/04/Pediatric-SOAP-Note.jpg

SOLUTION Nurs 6541pediatric Soap Note Studypool
https://sp-uploads.s3.amazonaws.com/uploads/services/734580/20210927184357_615210ed12ddf_nurs_6541pediatric_soap_notepage0.png
Sample Pediatric Soap Note - A Assessment Your analysis of the session If possible compare the patient s performance across sessions EXAMPLE Suzy s correct production of k in initial position increased from 60 in imitation and with a visual aid during the last session to 70 during today s session