Example Pediatric Soap Note Pediatric SOAP Note Example December 5 2018 Tim Fraticelli DPT MBA CFP This pediatric SOAP note example is based on an actual pediatric Physical Therapy evaluation Details have been edited to keep the identity of the patient confidential
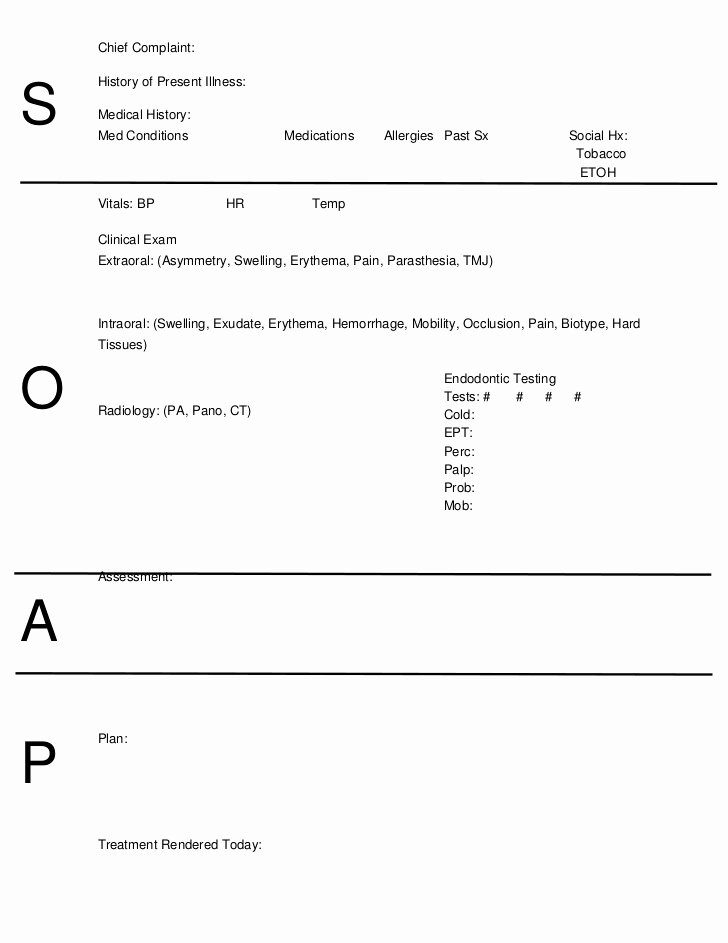
Learn how to write pediatric SOAP Notes Included are examples from SLPs that work with a pediatric caseload including articulation soap note examples Chief Complaint Reason or reasons for seeking medical attention To be recorded in informant s own words cough III History of Present Illness Chronological narration of client s present illness including the seven variables The patient s mother reports coughing x 1 2 days The symptoms have been moderate
Example Pediatric Soap Note
Example Pediatric Soap Note
https://markmeckler.net/wp-content/uploads/2019/11/pediatric-soap-note-template-elegant-7-essentials-to-writing-effective-pediatric-ot-soap-notes-of-pediatric-soap-note-template.jpg

Pediatric Soap Note Template Business
https://nationalgriefawarenessday.com/wp-content/uploads/2018/01/pediatric-soap-note-pac-5200-physical-diagnosis-iii-syllabus-3-728.jpg

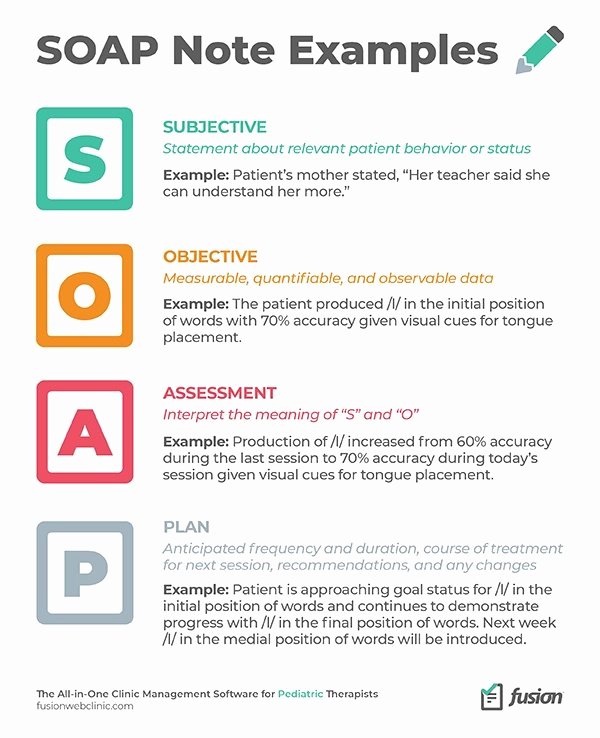
Pediatric Soap Note Template New Soap Note Examples Learn To Write Soap
https://i.pinimg.com/originals/24/2a/99/242a993b3f35d393ff75a10ec3e0924f.jpg
A Assessment Your analysis of the session If possible compare the patient s performance across sessions EXAMPLE Suzy s correct production of k in initial position increased from 60 in imitation and with a visual aid during the last session to 70 during today s session Occupational Therapy SOAP Note Example We ll cover each principle in detail below but first here are some SOAP note examples from an SLP in case you need a refresher 7 Principles for Improving your Pediatric OT Documentation SOAP Notes
SOAP Note Examples Example 1 Subjective 10 year old reports experiencing stomach pains for the last two days The mother adds that the child has had a loss of appetite and slight nausea but no vomiting Objective Abdominal exam shows tenderness in the lower abdomen no distension or rebound tenderness Here s info on pediatric SOAP notes including pediatric SOAP note examples which will be helpful for those in pediatric behavioral health
More picture related to Example Pediatric Soap Note
SOAP Note Examples 19 In PDF Examples
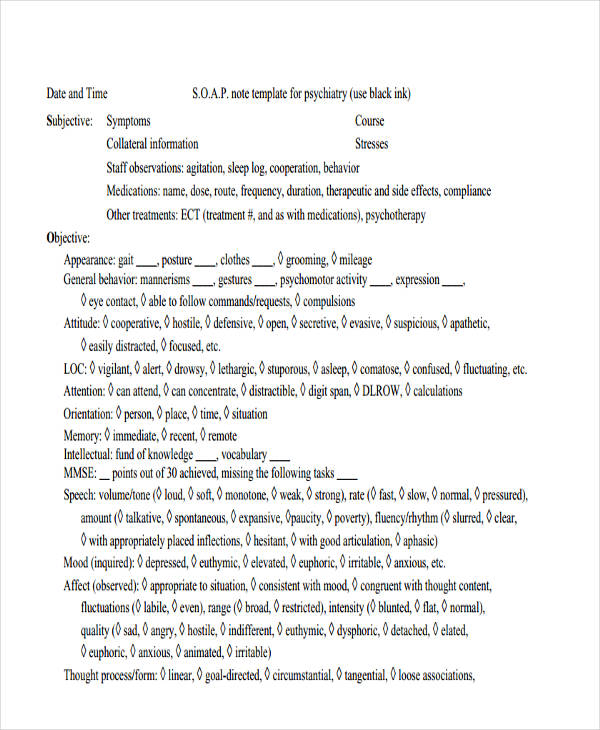
https://images.examples.com/wp-content/uploads/2017/04/Psychiatric-SOAP-Note-Example.jpg
40 Pediatric Soap Note Template Markmeckler Template Design
https://markmeckler.net/wp-content/uploads/2019/11/pediatric-soap-note-template-fresh-soap-notes-dentistry-word-of-pediatric-soap-note-template.jpg
FREE 15 SOAP Note Templates In PDF MS Word
https://images.sampletemplates.com/wp-content/uploads/2016/02/18143804/Pediatric-Soap-Note-Example.jpg
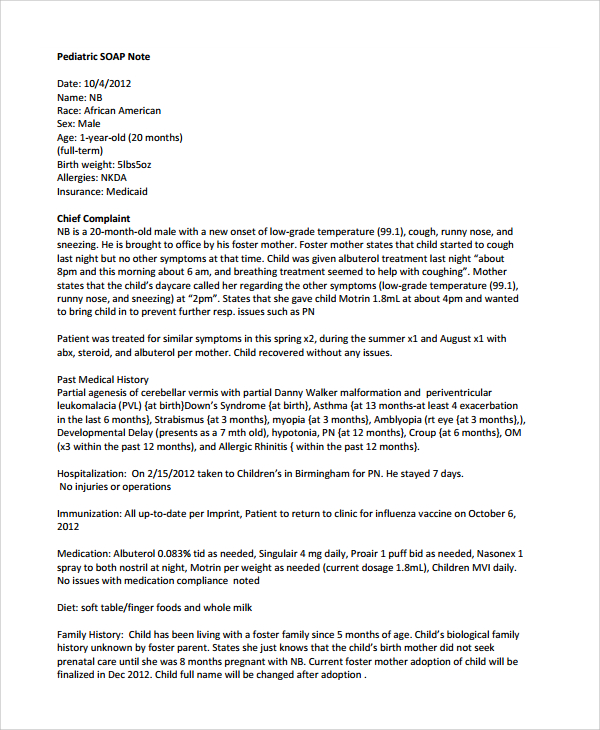
Pediatric SOAP Note Date 10 4 2012 Name NB Race African American Sex Male Age 1 year old 20 months full term Birth weight 5lbs5oz Allergies NKDA Insurance Medicaid Chief Complaint NB is a 20 month old male with a new onset of low grade temperature 99 1 cough runny nose and sneezing He is brought to office by his foster mother A pediatric SOAP note is a type of progress form used by pediatricians nurses and other healthcare professionals when assessing the health of a child It is based on the acronym SOAP which stands for Subjective Objective Assessment and Plan The note includes information gathered from the patient and or parent physical exam findings
General Pediatric Exams By SOAPnote posted 2010 11 26 updated 2023 02 22 Noteworthy Objective Exam Elements Pediatrics Cite Favorite 29 approximately 294 views in the last month View Skin Normal turgor and without lesions Eyes Red reflex present bilaterally Pupils equally round and reactive to light For example many infants under 6 months are easily managed on the examining table but from 8 months to 3 years you will usually have more success substituting the mother s lap Certain parts of the exam can sometimes be done more easily with the child in the prone position or held against the mother

SOAP Notes Occupational Therapy Examination Soap Note Occupational
https://i.pinimg.com/originals/62/3d/ec/623dec33aa213a8c4fddab01d151bb07.jpg

Pediatric Soap Note Template Lovely Free 19 Soap Note Examples In Pdf
https://i.pinimg.com/736x/d9/91/b7/d991b721f7f20ede228115f71673fa59.jpg
Example Pediatric Soap Note - SOAP Note Examples Example 1 Subjective 10 year old reports experiencing stomach pains for the last two days The mother adds that the child has had a loss of appetite and slight nausea but no vomiting Objective Abdominal exam shows tenderness in the lower abdomen no distension or rebound tenderness